Deeper Dive
I grew up surrounded by creativity. As a young kid, I loved crafts, painting, and music. As I grew and discovered my passion for science, that creativity remained a cornerstone of my identity. It underscores the projects I lead, especially in regards to research. That creativity enabled the formation of my project. Heart disease is the leading cause of death, and atherosclerosis (also called coronary artery disease, or CAD) is the most common form of cardiac disease, killing about 360,000 Americans each year. Though I have not had direct personal experience with heart disease, a heart attack killed my uncle, and I have been interested in cardiology since I was young. CAD is characterized by plaque buildup in coronary arteries, which restricts blood flow to the heart as arterial walls thicken and stiffen. The “gold standard” treatment for advanced forms of this disease is a surgery called a coronary bypass, in which the damaged artery is replaced by a graft from elsewhere in the body (usually the saphenous vein). Though this treatment has a high initial success rate, with time, the grafts often fail. Eight to ten years post-surgery, there is a 60% to 80% mortality rate increase. Further research has shown that the deaths are caused by the grafted cells’ behavior, as the vein cells accustomed to a low-pressure environment remodel to become thicker and stiffer. This metric is colossal, and the deaths are often blamed on heart disease, instead of the procedure. To fix this issue, research is being conducted to artificially create grafts that will not drastically remodel once in the body. They are called small-diameter tissue-engineered vascular grafts, or SD-TEVG, but their creation is not yet possible because not enough is known about how the vein cells remodel once in the arterial environment. This project takes a step back from developing grafts to learn more about cell behavior in a simulated arterial environment, thus providing the stepping stones necessary to create reliable, life-saving grafts. Additionally, this study utilizes new techniques. Prior to this experiment, polydimethylsiloxane (PDMS) had not been used to mimic pressure conditions typically found in the human body then used as substrates for human smooth muscle cells. It explores the intersections between physics, biology, and biomedical engineering, offering a new perspective that can save millions of lives on a global scale as it is built upon.
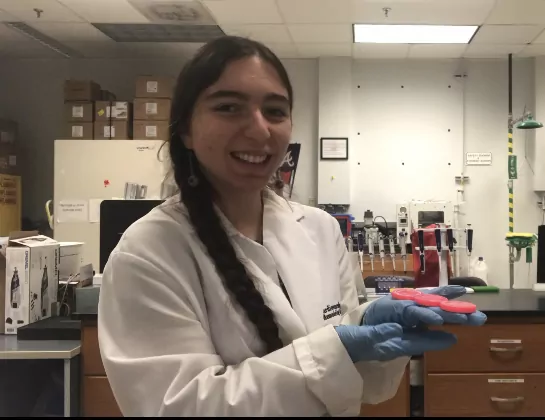
This study required team-work between multiple members of the lab, especially as I was too young to perform the BSL-2 cell work and had to receive an adult’s assistance in following the protocol I developed. Beyond having to find a mentor for the cell-work, I also struggled with some other difficulties while conducting this research. By the time I started my project, the majority of barriers imposed by COVID-19 had lessened. However, supply chain issues from the pandemic persisted, and the human venous smooth muscle cells ordered online took many extra weeks to ship due to lockdowns, labor shortages, and transportation issues. I also worked independently of my school, as the research class I was taking was terminated prior to my senior year. I had to balance the two schedules, sometimes spending my lunches in meetings and late evenings in the lab. However, doing so gave me a unique perspective, as I was often learning concepts in class then applying them to my project soon after. For instance, I was able to understand some formulas published on cell remodeling because I was taught what integrals were the week prior, and I learned about the structure of veins at school as I studied their cells’ biomechanical properties with the lab. Guidance from my teachers and mom both helped make this project possible; my biology teacher helped me become comfortable discussing my research in front of groups, and my mom helped me understand the scientific method when I was in elementary school and inspired me to be curious about the world. She has always been my biggest supporter, and I am immensely grateful for her love and dedication.
I see my work enabling the research that can save some of the hundreds of thousands of people who die due to CAD each year. Using the data gathered in this study, researchers can predict the changes cells undergo after being autotransplanted during coronary bypasses and account for them in their SD-TEVG designs. This will lead to SD-TEVG that are engineered to not drastically remodel once implanted, thus preventing the surgeries from failing.