Deeper Dive
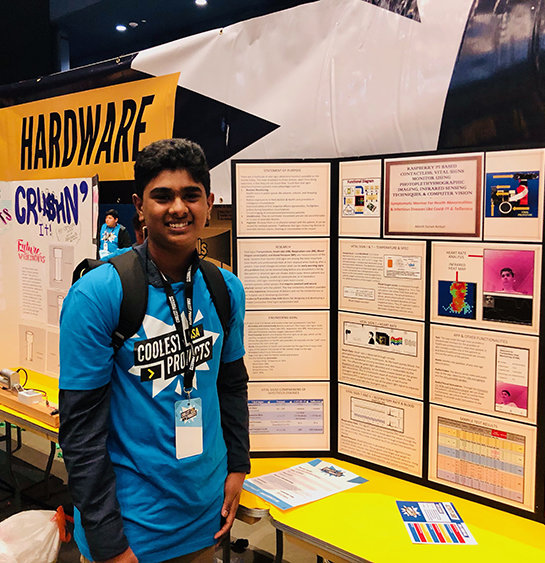
When I was in middle school, my mother suffered from unexplainable blackouts for six months that culminated in a 3rd-degree heart block. I was distraught to see my fiercely independent mother lying limp on a hospital bed helplessly hooked up to countless vital signs monitors. Unable to do anything to help her, I was overwhelmed by a sense of despair. After my mother expressed how being tethered to monitors made her feel even more helpless and depressed, I was inspired to build a completely contactless vital sign monitor that does not hinder a patient's movements. Later, during the Ebola and Zika outbreaks, reading about the risk that frontline healthcare providers faced further strengthened my desire to develop this contactless device. When I first started building the prototype, I focused on just the heart rate and body temperature detection functionalities. When the COVID-19 pandemic took the world by surprise, my device became all the more relevant as it can reduce exposure to front line workers through its remote, contactless monitoring features. Furthermore, as SpO2 (blood oxygen levels) and respiratory rates are important factors physicians consider when diagnosing and caring for COVID-19 patients, I improved the device by adding SpO2 and respiratory rate monitoring features.
While working on this project, I encountered several technical and non-technical challenges. The main technical challenges involved the development and implementation of heart rate and blood pressure detection. At first, the accuracy of the heart rate detection fluctuated wildly—after periods of being extremely accurate, the program would erroneously report a heart rate of 60 bpm. After careful evaluation of test results, I ruled out several factors that I initially thought were affecting the accuracy of the measurement, including image resolution, patient background, and participant skin tone. After much troubleshooting, I found the primary reason for the erroneous 60 bpm reading was the frequency of artificial light, which flickers at a constant interval. This constant interval is the strongest signal in the composite wave, so after the Fast Fourier Transform Technique, the program selected this signal as the heart rate. I overcame this problem by testing in natural light. My main non-technical challenge and the most difficult aspect of my project was recruiting volunteers to test my prototype. The process of enlisting the 48 candidates taught me the importance of clear and succinct communication. I learned to sell the importance of the project so that candidates would be more likely to volunteer their time and effort. I also had to overcome hurdles including assuring volunteers that the testing process was safe as the device is entirely contactless. Though difficult, the testing process proved very valuable because the participants provided great feedback from a user experience standpoint. As I conducted numerous iterations of developmental and testing phases, this experience taught me that the success of any form of research requires continued persistence despite challenges. Next, while I worked independently for most part, I received a lot of guidance from my brother, Vardhaan Sai Ambati and Johan Sosa, my mentor, DIY Biologist, & BioCurious Member. They helped me understand complicated research papers, provided debugging tips when I hit a roadblock, offered constructive critiques of my approach, and monitored me during testing. Members of BioCurious helped me troubleshoot coding issues, and Mrs. Thuy-Anh Nguyen, my high school Advanced Science Research Director, helped me prepare presentation material. While I received help from many different people, my school’s Biology teacher, Mr. Tom Motroni, provided the essential foundation of my biotechnology background. Finally, regarding the pandemic, I believe that it actually helped me improve my project. Although it did make it difficult for me to contact mentors or to gather participants for my trial, the environment it created acted as a catalyst, pushing me to increase the capabilities of the device, adding other vital signs monitors and even an app for long distance monitoring.
I believe that my project fills a true need. The device is a continuous and contactless monitor of all five vital signs that forms a comprehensive health picture of a patient. This vital signs monitor has four main features that demonstrate its unique ability to transform the healthcare industry and allow for significant contributions to society. First, the detection of the five vital signs allows healthcare workers to quickly create a comprehensive health profile of the patient. While there are already available vital signs monitors, most are not contactless and do not monitor all five major vital signs. Furthermore, the COVID-19 pandemic taught us the necessity of monitoring blood oxygen levels (SpO2) and respiratory rate along with body temperature and heart rate to detect symptoms of infectious diseases, making this particular aspect of my device all the more important. In addition, monitoring vital signs can alert caretakers quickly if anything abnormal occurs in patients such as in Sudden Infant Death Syndrome, which tragically kills 1 in a 1000 babies each year. Second, the contactless feature can provide invaluable protection against diseases to frontline healthcare workers. According to Kaiser Health News and the Guardian, over 2900 healthcare workers died from COVID-19 this past year due to exposure to infected patients. This device can protect this vulnerable yet essential class of workers because it reduces the likelihood that these workers are exposed to hazardous and/or contagious materials. Third, the contactless, continuous monitoring capability of the device ensures the comfort of patients both in hospitals and in home care settings. Comfortable monitoring is especially important for vulnerable demographics like infants, ill patients, and the elderly as evidenced by my mother’s own experience at the hospital. Fourth, while traditional patient vital signs monitors with continuous capabilities can cost upwards of $1000, this device costs just ~$130. The low cost of the device can help bolster the home healthcare system, and more people can utilize continuous monitoring technologies as it is much more accessible. In addition, my project has the potential to diminish the strain on the healthcare system and reduce overall healthcare costs. Especially in cases like the COVID-19 pandemic, this low-cost device can be used by healthcare workers to quarantine patients at home, while still monitoring their health— preventing hospitals from being overwhelmed, reducing healthcare costs, and limiting exposure (potentially saving the lives of frontline healthcare workers)!